Broward Eye Care Keratoconus Diagnosis And Management Expertise
The doctors’ experience has allowed thousands of keratoconic patients to achieve clear vision, when less experienced lens fitters had failed. Broward Eye Care receives referrals for the treatment of keratoconic patients from throughout the United States and South America.
The term keratoconus is derived from two Greek words: “kerato”, meaning cornea, and “konos”, meaning cone. Keratoconus is a disease of the cornea in which the cornea looses its natural round shape and becomes distorted with cone-like bulging, progressive thinning, and associated reduction in vision quality.
Keratoconus is a progressive disease that can range from very mild to very severe. The progression is generally slow and may stop at any stage. Keratoconus is one of a group of corneal degenerations that is characterized by corneal thinning. These conditions are termed “Ectasias” of the cornea.

What Causes Keratoconus?
Although we have been aware of keratoconus for over two hundred years, we are still not certain about the cause of keratoconus. We are fairly certain that it is genetically programmed and family history is a risk factor. About 7% of patients with keratoconus have known relatives with the disease.
Generally speaking, there is about a 1 in 10 chance of a patient with keratoconus having an offspring with the disease (unless there is evidence of keratoconus in successive generations, which increases the probability level).
Additionally, there may be links to the endocrine (hormonal) system in that keratoconus tends to appear in its early stages at puberty. Associations with allergy (“atopy”) are common as well. Currently there are a number of studies going on in terms of determining the underlying causes and associations of and with keratoconus.
The incidence of keratoconus is not well known, but an approximation is that about 1 in 2,000 persons in the general population have keratoconus. This is a relatively high number in terms of disease rates. Keratoconus is a relatively common eye disease.
Diagnosing Keratoconus
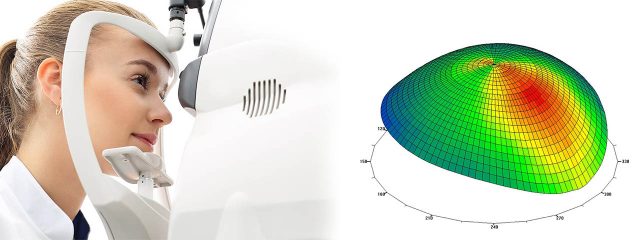
With new technologies that measure the shape and thickness of the cornea in exquisite detail, we are now able to detect the presence of keratoconus well before subjective symptoms develop. Corneal Topography has become the standard of care in diagnosing keratoconus.
A computerized system images the shape of the cornea by taking tens of thousands of data points from the corneal surface. The results are instantly analyzed and a topography map is generated. The colors of the map correspond to the shape of the cornea.
In keratoconus the cornea tends to be very steep in shape and quite irregular in shape. Quantitatively the topography values can be monitored for change over time to determine if the condition is progressive. Broward Eye Care is proud to use the state of the art corneal topography and analysis system in the world today, Oculus Keratograph Corneal Analysis.
At some point in the disease process your doctor will note visible thinning of the cornea under the biomicroscope along with folds in the cornea (called “striae”). Other clinical signs include the deposition of iron in the cornea (“Fleisher’s Rings”), corneal scares, large increases in astigmatism, and reduced correctable vision with glasses. Patients complain of distortion and progressive blur of their vision along with large and frequent changes in their prescription.

Get Treatment From Our Keratoconus Specialist
During the very early stages of keratoconus, conventional eyeglasses can correct the mild myopia (nearsightedness), and astigmatism that develops.
At these stages vision is often correctable to 20/20. As the disease progresses a loss of best corrected glasses vision occurs. It is then that special keratoconus contact lenses are required to achieve clear vision.
The contact lenses function to “mask” the irregularity of the corneal surface, thus increasing the quality of vision in comparison to the vision through glasses. For many years the only method to correct vision well in keratoconus was with the use of hard contact lenses and then eventually rigid gas permeable contact lenses.
Today gas permeable contact lens correction of keratoconus is still the mainstay of treatment, however very specialized designs have been developed that improve vision and comfort far beyond yesterdays lenses.
In addition, customized soft lenses, hybrid, and scleral lenses can now be designed that can also provide excellent visual results in many cases of keratoconus. Some of the highly customized designs used by your contact lens specialists at Broward Eye Care include among many others:
- KBA bi-aspheric (gas perm)
- Rose-K designs (gas perm)
- IKone bi-aspheric (gas perm)
- McGuire designs (gas perm)
- Soper designs (gas perm)
- HydraKone (soft lens)
- AlterKone (soft lens)
- Synergeyes Clear Kone and SynergEyes KC (hybrid soft and gas perm combination)
- Ultrahealth (hybrid soft and gas perm combination)
- Atlantis (sclera gas perm)
- Zenlens (sclera gas perm)
- Onefit (sclera gas perm)
- Intra-Limbal design (large diameter gas perm)
- “Piggy-back” lens systems (combinations of soft disposable lenses and gas permeable lenses fit over the soft lens for improved comfort and fitting)

Surgical Treatments For Keratoconus Specialist In Fort Lauderdale, FL
Cornea Transplant
Less than 10% of patients with keratoconus progress to the point where contact lens treatment is insufficient to correct vision adequately or contact lens intolerance develop.
These patients require some form of corneal transplantation. Eye banks in most major cities have a great supply of corneas for transplantation, so waiting on a recipient list is generally a thing of the past.
Corneal transplantation is one of the most successful forms of organ transplantation. Rejection of corneal tissue is relatively infrequent and is very successfully managed with topical medication eye drops. The outcome for corneal transplantation in cases of keratoconus is very good.
Following corneal transplants, most patients do require glasses and often contact lenses for proper visual correction. Should any of our keratoconus require corneal transplantation, your doctor will make the most appropriate referral for you.
INTACS for Keratoconus is small arc shape implants that can be surgically placed within the corneal tissue to effect a purposeful change in the surface shape of the cornea. Initially developed for the correction of myopia (nearsightedness), doctors began to utilize Intacs for certain cases of keratoconus to provide a relatively more regular front surface. This allows for some degree of improvement in vision and in some instances, more stable contact lens fitting. There are certain specific criteria that make a patient with keratoconus a candidate for Intacs. Your keratoconus specialist at Broward Eye Care is able to make that determination.
Collagen Cross Linking With Riboflavin
Collagen Cross-linking with Riboflavin (C3-R) New research indicates that keratoconus may be treated with a procedure called Corneal Collagen Cross-linking with Riboflavin (C3-R®). This is a new treatment that increases the stiffness and rigidity of the cornea and stabilizes ectasia. Some patients who previously had progressive ectasia have now been treated and followed for up to five years without evidence of any further change in their condition. At present, it is not known whether the stabilizing effect of C3-R® on keratoconus is permanent, but the C3-R® treatment could potentially be repeated if it was necessary. The bulk of the cornea is made from collagen fibers which are arranged in bundles. The strength and rigidity of the cornea are partly determined by how strongly the fibers are linked together. Over the course of a lifetime, the cornea becomes progressively stiffer due to natural cross-linking between the fibers. Riboflavin (vitamin B2) is a naturally occurring compound which strongly absorbs UV light. By applying riboflavin to the cornea at the same time as exposing it to a UV light source, the riboflavin not only enhances the cross-linking effect of the UV light, but also absorbs the light to an extent that the inner layers of the cornea and intra-ocular structures are protected from the potentially damaging effects of the light rays. Studies are currently taking place which are evaluating the safety and efficacy of C3-R for keratoconus. The hope is the C3-R may allow us to slow down or halt the progression of the disease.
Website Links For Keratoconus
- National Keratoconus Foundation MDJunction.com (Support Group)
- UK Keratoconus Self Help and Support Association

